FAQ on UDI, Part 1: Facts About the Unique Device Identification Directive
Following the Unique Device Identification directive (UDI), mandated by the Food & Drug Administration (FDA), medical devices have to be clearly identified to ensure traceability and patient safety. The rule-compliant implementation challenges medical device manufacturers and raises many questions.
What is the reason for the implementation of UDI?
The UDI system addresses all of the following aspects:
- More efficient product recalls.
- Improved counterfeiting protection.
- Simplification of data entry and accessibility with different systems.
- Security throughout the entire supply chain.
- Field Safety Corrective Action – FSCA.
- Better identification, documentation and prevention of incidents.
- Prevent medical errors from occurring.
Additionally, the labeling system enables the simplification of logistics, ordering and delivery processes.
Is laser marking suitable for marking UDI codes?
For the requirement of direct part marking, laser marking, especially on plastic and metallic devices, appears to be the only technology that is able to pass passivation processes while guaranteeing long-lasting marks that can resist high wear and abrasion as well as frequent sterilization cycles. In order to meet the labeling requirements, laser markings must be of high contrast, precise, long lasting, able to fit into small spaces and must not affect the surface finish of the device negatively. How fiber laser markers create corrosion-resistant markings on medical products, is shown in a representative study about “Laser marking of reusable surgical instruments mastering multi-process requirements".
As the marking takes place at the end of the production cycle, scrap must be kept to a minimum and repeatable results and process stability are imperative. For a reliable identification, vision-based laser marking has become the chosen technology: It enables both a safe marking as well as a lean production.
How vision-based laser marking helps to mark UDI codes reliably and efficiently
A vision-based laser marking workflow, like HELP (Holistic Enhanced Laser Process), helps facilitate and streamline the marking process. An integrated camera ensures process reliability before, during and after laser marking. HELP is a three-staged closed-loop medical device marking process. Prior to marking, the right parts are validated, then the marking position is automatically aligned with the part so that only the correct mark will be applied in the correct position. Finally, the integrated vision also verifies the marked contents. Utilizing this approach, scrap due to marking errors can be reduced by up to 80 percent.
Although many manufacturers are requested to implement several essential modifications in their production process, one can assume that the traceability of medical devices will pay off in the end. Not only for the safety of patients, but also for streamlining the companies’ manufacturing and logistics supply chain. Laser marking with integrated vision appears to be a sustainable and economic solution in response to the actual marking requirements.
UDI in the U.S. and in Europe: Where does the directive apply?
The goal of the UDI system is to increase patient safety and to allow for a sustainable traceability. The FDA-directive applies to medical devices that are produced or imported and are distributed in the U.S. Equivalent directives are being introduced internationally: The European Union has just released a resolution on UDIs within the Medical Device Regulation (MDR), becoming effective gradually from 2020 on.
Both systems have in common the central allocation and registration of product numbers in a common database. The center of the American UDI system is the “Global Unique Device Identification Database” (GUDID), which acts as a registry and as a reference catalog for every device with an identifier. The European equivalent is EUDAMED (European Database on Medical Devices).
What is the structure of a UDI code?
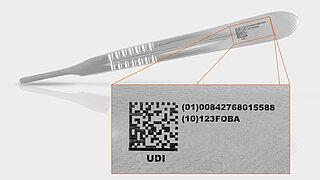
UDI codes consist of a Device Identifier (DI) and a Production Identifier (PI), the first of which identifies the manufacturer/labeler and the specific version or model of the device (also reference code). The Device Identifier is a globally unique product code which allows the clear identification of a device and must be entered in the central registry. The Production Identifier is optional and represents the variable portion of a UDI that identifies variables like the lot and batch numbers, serial numbers, expiration or manufacturing dates etc.
According to 21 CFR 801.40, medical devices have to carry a UDI that is represented in two forms:
- Easily readable plain-text (HRI/Human Readable Interpretation), alpha-numeric characters
- AIDC technology (Automatic Identification and Data Capture), which means a machine readable code (barcode/2D code)
In case the UDI code is applied as a permanent direct mark, it must be in either or both (1) easily readable plain-text and (2) AIDC form or alternative technology (see 21 CFR 801.45).
UDI marking on stainless steel umbilical cord scissor. Marking procedure: Annealing with a fiber laser marker.
GS1, HIBC, ICCBBA: Which code is suitable for UDI marking?
The FDA has accredited three organizations as UDI issuing agencies: GS1, HIBCC (Health Industry Business Communications Council) and ICCBBA (International Council for Commonality in Blood Banking Automation). Both the Health Industry Bar Code (HIBC) and the GS1 code are equally suitable for the UDI compliant marking of medical products and devices. The ICCBBA UDI code, as approved by the FDA, is best adapted to identify products of human origin (like plasma or transplants).
UDI codes are graphically depicted in an assembly of two forms: a human readable plain text of alpha-numeric characters and a machine-readable code (see above). There are different forms of machine readable codes available: The GS1-128 linear bar code, the GS1 data matrix code from GS1, the HIBC linear bar code and the HIBC data matrix code, and the linear ISBT 128 and 2D code from ICCBBA. Depending on the accredited issuing agency, each product can receive its unique code in any of the above formats.
UDI code examples
Which technology is suitable for UDI-compliant marking?
One of the major challenges facing UDI is the implementation of the appropriate direct marking technology. The FDA does not specify which of the various available options should be used. Moreover, not every method is suitable for secure and UDI-compliant direct part marking; therefore choosing the best method to meet the requirements can be difficult and is crucial.
Laser marking is ideally suited for the direct marking of medical devices with the Unique Device Identifier. It fulfills all the criteria relevant for safe product marking based on medical standards and UDI requirements. The laser produces high-quality, permanent, readable markings on products as well as packaging and ensures the highest precision and process stability when combined with integrated vision systems.
FDA compliance dates: Which products have to be marked with a UDI code as from when?
Where and when a UDI code has to be applied to a product depends on its risk class and intended use. The UDI system differentiates between the marking of the packaging of labels and direct marking on the product. If the product is reused and/or reprocessed before each use, the UDI marks need to be directly applied on the device. The last deadline for the marking of packaging and labels will be reached in 2018. At that point, the packaging and labels of all class I – III products must carry a UDI code in plain text and machine-readable form, using automatic identification and data collection (AIDC) technology.
The FDA has defined three risk classes, based on the degree of control needed to guarantee the safety and effective use of the products.
- Class I (low risk, general controls): e.g. bandages, stethoscopes, surgical scissors, dental floss, mechanical wheelchairs.
- Class II (moderate risk, general and specific controls): e.g. infusion pumps, surgical sutures, bone screws, syringes, condoms, powered wheelchairs.
- Class III (high risk, general controls and premarket approval, life-saving and life-sustaining): e.g. heart valves, knee prosthesis, pacemakers, automated external defibrillators.
The UDI marking compliance deadlines are phased in stages based on product risk classifications. Codes must be applied on labels and packages or on the product itself (Direct Part Marking DPM). According to the FDA, DPM is required for implants and devices intended to be reprocessed or reused over an extended period of time (several months or years). The permanent marking is required as it is expected that such devices will be separated from their original packages.
The compliance deadlines of the FDA regarding Direct Part Marking (for devices that are intended to be used more than once and intended to be reprocessed before each use) are as follows:
- 2015: Implantable, life-saving, life-sustaining products.
- 2016: Class III products.
- 2018: Class II products.
- 2020: Class I products.
(Visit the FDA-website for more details and latest information.)
A directly marked UDI code is only required if the corresponding products are processed, for example cleaned, sterilized or passivated, before their use. Even products that do not necessarily have to bear a directly marked code (like sterile packaged implants for single use) get marked for functional reasons and fraud prevention.